Practice Essentials
Venous thromboembolism (VTE) encompasses two interrelated conditions that are part of the same spectrum, deep vein thrombosis (DVT) and pulmonary embolism (PE) (see the image below). The spectrum of disease ranges from clinically unsuspected to clinically unimportant to massive embolism causing death.
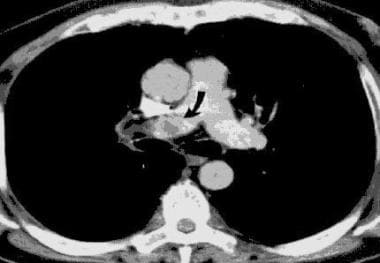 Venous Thromboembolism (VTE). Helical CT scan of the pulmonary arteries. A filling defect in the right pulmonary artery is present, consistent with a pulmonary embolism.
Venous Thromboembolism (VTE). Helical CT scan of the pulmonary arteries. A filling defect in the right pulmonary artery is present, consistent with a pulmonary embolism.
Signs and symptoms
Signs and symptoms of thromboembolism include the following:
-
Acute onset of shortness of breath; dyspnea is the most frequent symptom of PE
-
Pleuritic chest pain, cough, or hemoptysis (with a smaller PE near the pleura)
-
Syncope (with a massive PE)
-
Sense of impending doom, with apprehension and anxiety
-
Complaints related to signs of DVT, lower-extremity swelling, and warmth to touch or tenderness
-
Tachypnea (respiratory rate >18 breaths/min)
-
Tachycardia
-
Accentuated second heart sound
-
Fever
-
Normal findings from lung examination
-
Cyanosis
See Presentation for more detail.
Diagnosis
Workup for thromboembolism includes the following:
-
Pulmonary angiography: Diagnostic standard for PE
-
Ventilation-perfusion scanning: Most common screening technique
-
Venography: Standard test for validating new diagnostic procedures
-
Arterial blood gas values on room air: Hypoxemia, elevated alveolar-arterial oxygen gradient
-
Acid-base status: Respiratory alkalosis
-
Enzyme-linked immunoassay (ELISA) for D-dimer
-
Electrocardiography, especially for ruling out myocardial infarction
-
Chest radiography: Most often normal but occasionally suggestive
-
Helical (spiral) computed tomography of pulmonary vessels
-
Doppler ultrasonography of venous system
-
Echocardiography
-
Impedance plethysmography: Of limited value when DVT is asymptomatic or distal or when findings are nonocclusive
See Workup for more detail.
Management
Anticoagulant medications include the following:
-
Heparin or a low-molecular-weight heparin (LMWH)
-
Subsequent administration of an oral coumarin derivative (typically, warfarin sodium)
-
Oral factor Xa inhibitors (eg, rivaroxaban)
Thrombolytic options (for initial treatment of patients with acute, massive PE causing hemodynamic instability) include the following:
-
Tissue plasminogen activator (t-PA; first-choice thrombolytic agent), including the recombinant agents alteplase, reteplase, and tenecteplase
-
Streptokinase (risk of antibody development)
-
Urokinase (of limited availability)
Surgical interventions include the following:
-
Thrombectomy
-
Embolectomy (limited to massive PE when thrombolysis is contraindicated or other treatments have failed)
-
Venous interruption (currently rare)
Prevention
Thromboprophylaxis reduces the incidence of DVT and fatal PE and may be achieved by pharmacologic or mechanical means. Medications used for prevention of thromboembolism include the following:
-
Unfractionated heparin
-
LMWH
-
Danaparoid
-
Warfarin
-
Direct oral anticoagulants
-
Aspirin
Mechanical approaches to thromboprophylaxis include the following:
-
External compression
-
Early ambulation
See Treatment and Medication for more detail.
Background
Venous thromboembolism (VTE) encompasses two interrelated conditions that are part of the same spectrum, deep venous thrombosis (DVT) and pulmonary embolism (PE). PE is the obstruction of blood flow to one or more arteries of the lung by a thrombus lodged in a pulmonary vessel, as shown in the image below. (See Pathophysiology and Etiology.)
PE and DVT can occur in the setting of disease processes, following hospitalization for serious illness, or following major surgery. In 1856, Virchow demonstrated that 90% of all clinically important PEs result from DVT occurring in the deep veins of the lower extremities, proximal to and including the popliteal veins. However, emboli also can originate from the pelvic veins, the inferior vena cava, and the upper extremities. (See Pathophysiology, Etiology, Presentation, and Workup) [1, 2, 3, 4, 5]
Thromboembolic disease is the third most common acute cardiovascular disease, after cardiac ischemic syndromes and stroke. The spectrum of disease ranges from clinically unsuspected to clinically unimportant to massive embolism causing death, and indeed DVT and PE frequently remain undiagnosed because they may not be suspected clinically. Untreated acute proximal DVT causes clinical PE in 33-50% of patients. Untreated PE often is recurrent over days to weeks and can either improve spontaneously or cause death. (See Epidemiology, Presentation, and Workup.)
In a study of Virchow's triad in "silent" DVT, Lurie et al assessed 152 patients who underwent venous stenting for proximal venous outflow obstruction and who had routine hypercoagulation profile testing performed preoperatively. [6] By history or intraoperative chronic postphlebitic changes (CPPCs), 77 patients (50.7%) were positive for remote DVT; 51 (33.6%) had intraoperative findings of CPPCs without a history of DVT; 20 (13.2%) had intraoperative CPPCs with a history of DVT; and six (3.9%) had a history of DVT without intraoperative findings. Findings of CPPCs were significantly increased among patients with a history of DVT, and intraoperative findings of CPPCs were significantly increased in patients with one or more positive hypercoagulation markers.
Guidelines
Guidelines for the diagnosis and management of VTE have been published by the American Society of Hematology, the American Society of Clinical Oncology (ASCO), the European Society of Anesthesiology (ESA), the American College of Chest Physicians (ACCP), the American Academy of Orthopaedic Surgeons (AAOS), and the International Initiative on Thrombosis and Cancer (ITAC). Go to Guidelines for more information.
AAOS guidelines
The 2011 guidelines from the American Academy of Orthopaedic Surgeons (AAOS) on preventing VTE in patients undergoing elective hip and knee arthroplasty included the following recommendations [7, 8] :
-
Recommend against routine postoperative duplex ultrasonography screening
-
Assess risk of previous VTE
-
Assess risk for bleeding
-
Suggest discontinuance of antiplatelet agents before undergoing elective hip or knee arthroplasty
-
Suggest pharmacologic agents and/or mechanical compressive devices for prevention of VTE in those undergoing elective hip or knee arthroplasty who are not at elevated additional risk for VTE or bleeding
-
Pharmacologic prophylaxis and mechanical compressive devices for those who have had previous VTE and are undergoing elective hip or knee arthroplasty
-
Mechanical compressive devices for those who have had known bleeding disorder and/or active liver disease and are undergoing elective hip or knee arthroplasty
-
Patients should undergo early mobilization following elective hip and knee arthroplasty
-
Use of neuraxial anesthesia for those undergoing elective hip or knee arthroplasty to help limit blood loss
-
No recommendation can be made for or against the use of inferior vena cava (IVC) filters
Other guidelines
A study by Khokhar et al indicated that there is a lack of uniformity among venous thromboprophylactic guidelines for elective knee arthroplasty. Reviewing 12 guidelines, the investigators found that although almost all of them advocated the use of LMWH and fondaparinux (a synthetic, pentasaccharide anticoagulant), recommendations for other drugs varied, as did drug dosages, duration, and recommendation grades. [9]
In an article addressing the differences between the antithrombotic guidelines of the American College of Chest Physicians (ACCP) and those of the AAOS, the authors noted that recommendation variations were based on methodology and evidence differences. [10] With updates to these two more popular VTE guidelines, similar recommendations were offered that focus on minimizing symptomatic VTE and bleeding complications. [11]
Pathophysiology
A thrombus is a solid mass composed of platelets and fibrin with a few trapped red and white blood cells that forms within a blood vessel. Hypercoagulability or obstruction leads to the formation of a thrombus in the deep veins of the legs, pelvis, or arms.
As the clot propagates, proximal extension occurs, which may dislodge or fragment and embolize to the pulmonary arteries. This causes pulmonary artery obstruction, and the release of vasoactive agents (ie, serotonin) by platelets increases pulmonary vascular resistance. The arterial obstruction increases alveolar dead space and leads to redistribution of blood flow, thus impairing gas exchange due to the creation of low ventilation-perfusion areas within the lung.
Stimulation of irritant receptors causes alveolar hyperventilation. Reflex bronchoconstriction occurs and augments airway resistance. Lung edema decreases pulmonary compliance. The increased pulmonary vascular resistance causes an increase in right ventricular afterload, and tension rises in the right ventricular wall, which may lead to dilatation, dysfunction, and ischemia of the right ventricle. Right heart failure can occur and lead to cardiogenic shock and even death. In the presence of a patent foramen ovale or atrial septal defect, paradoxical embolism may occur, as well as right-to-left shunting of blood with severe hypoxemia.
Etiology
Risk factors for thromboembolic disease can be divided into a number of categories, including patient-related factors, disease states, surgical factors, and hematologic disorders. Risk is additive.
Patient-related factors include age older than 40 years, obesity, varicose veins, the use of estrogen in pharmacologic doses (ie, oral contraceptives or hormone replacement therapy), and immobility.
Disease states such as malignancy, congestive heart failure, nephrotic syndrome, recent myocardial infarction, inflammatory bowel disease, spinal cord injury with paralysis, and pelvic, hip, or long-bone fracture confer increased risk of thromboembolic disease.
Surgical factors are related to procedure type and procedure duration. Among patients who have undergone hip surgery, 50% have a proximal DVT on the same side as the hip surgery. This is thought to be due to a twisting of the femoral vein during total hip replacement. The incidence of DVT is higher in patients who have undergone knee surgery. [9]
In a study of patients following pelvic surgery, 40-80% had calf DVT, and 10-20% had thigh vein thromboses. Fatal PE developed in 1-5% of patients. The risk for thromboembolic disease has been shown to be increased with coronary artery bypass grafting (CABG), urologic surgery, and neurosurgery. [12]
One study identified the following four risk factors as being highly predictive of VTE among hospitalized medical patients [13] :
-
Previous VTE
-
An order for bed rest
-
Peripherally inserted central venous catheterization line
-
Cancer diagnosis
This four-element risk assessment model was accurate at identifying patients at risk of developing VTE within 90 days and was more effective than the Kucher Score, a risk assessment score. [13]
Hematologic disorders that increase thromboembolic risk include the following:
Activated protein C resistance (factor V Leiden)
-
Prothrombin mutation [14]
Risk prediction algorithm
A prospective, open cohort study developed a new clinical risk prediction algorithm (QThrombosis) to assess the risk of VTE development. Using routinely collected data from 564 general practices in England and Wales, this study found that independent predictors at 1 and 5 years included the following [15] :
-
Age
-
Body mass index
-
Smoking status
-
Hospital admission in past 6 months
-
History of varicose veins
-
Congestive cardiac failure
-
Chronic renal disease
-
Cancer
-
Chronic obstructive pulmonary disease
-
Inflammatory bowel disease
-
Current prescriptions for antipsychotic drugs
Oral contraceptive use, tamoxifen use, and hormone replacement therapy were noted in the study as independent predictors in women. This risk assessment can help to identify patients at high risk for VTE and may help determine a course of treatment.
Epidemiology
United States statistics
The Centers for Disease Control and Prevention (CDC) estimated that over a 3-year period (2007-2009), there was an estimated annual average of 547,596 hospitalizations in which VTE was diagnosed, for patients aged 18 years or older. [16, 17]
Over the same period, for the same age group, an estimated average of 348,558 hospitalizations in which DVT was diagnosed occurred annually, and an estimated average of 277,549 hospitalizations in which PE was diagnosed occurred annually. Among these patients, an estimated average of 78,511 hospitalizations in which both DVT and PE were diagnosed occurred annually.
International statistics
Thromboembolism has a significant impact on morbidity and mortality internationally. A multinational report of European Union countries estimated that the total number of symptomatic, nonfatal VTE events per annum was more than 465,000 cases of DVT and more than 295,000 cases of PE. The authors estimated more than 370,000 VTE-related deaths, of which 7% were diagnosed ante mortem and 34% were sudden fatal PE. [18]
Age-, sex-, and race-related demographics
Age is a risk factor for thromboembolic disease, being greater in older patients than in younger ones. The risk doubles with each decade in persons older than 40 years.
According to the CDC, the estimated annual average number (for years 2007-2009) of hospitalizations in which VTE was diagnosed was as follows for specific adult age groups [17] :
-
Aged 18-39 years - 54,034
-
Aged 40-59 years - 143,354
-
Aged 60 years or older - 350,208
The estimated annual average rate (for years 2007-2009) of hospitalizations in which VTE was diagnosed was as follows for specific adult age groups:
-
Aged 18-39 - 60/100,000 population
-
Aged 40-49 - 143/100,000 population
-
Aged 50-59 years - 200/100,000 population
-
Aged 60-69 years - 391/100,000
-
Aged 70-79 years - 727/100,000
-
Aged 80 years or older - 1134/100,000
According to the CDC, the estimated average annual number (for years 2007-2009) of hospitalizations in which VTE was diagnosed was as follows for adult males and females [17] :
-
Males - 250,973
-
Females - 296,623
The incidence of thromboembolism is higher in African Americans than it is in whites, whereas Asians have a lower incidence than do African Americans and whites. PE occurs more frequently in males than in females.
Prognosis
Thromboembolic disease accounts for approximately a quarter of a million hospitalizations in the United States annually and for about 5-10% of all deaths.
About one third of PE cases are fatal. Of these, 67% are not diagnosed ante mortem, and 34% occur rapidly. A high rate of clinically unsuspected DVT and PE leads to significant diagnostic and therapeutic delays, and this accounts for substantial morbidity and mortality.
Studies demonstrate a 95% risk reduction with treatment of thromboembolic disease. There is, however, a risk of recurrence following the discontinuance of treatment that is related to the type and number of risk factors the patient has and whether they persist following completion of treatment. Some 5-7% of all recurrences are fatal.
Patient Education
For the success and ease of outpatient treatment, patients on oral warfarin anticoagulation should be instructed on the impact of dietary choices on treatment goals and the need for frequent monitoring. Instruction on the avoidance of reversible risk factors would be helpful in preventing disease recurrence.
The best approach to patient education is one that starts with open communication with the patient and family, reviewing not only the procedure or planned surgical intervention, but also potential complications.
For patient education information, see the Lungs Center, as well as Pulmonary Embolism, Deep Vein Thrombosis (Blood Clot in the Leg, DVT), and Blood Clots.
-
Venous Thromboembolism (VTE). Pulmonary embolism within the pulmonary artery.
-
Venous Thromboembolism (VTE). Ventilation-perfusion scan. Left image: Posterior view of normal findings on ventilation scan. Right image: Posterior view of a perfusion scan that reveals a perfusion defect in the left upper quadrant. The defect in the middle of the image is due to the position of the heart.
-
Venous Thromboembolism (VTE). Helical CT scan of the pulmonary arteries. A filling defect in the right pulmonary artery is present, consistent with a pulmonary embolism.
Tables
What would you like to print?
- Overview
- Presentation
- DDx
- Workup
- Treatment
- Guidelines
- Venous Thrombosis Clinical Practice Guidelines (ESVS, 2021)
- ASH Updated Recommendations for Management of VTE (2020)
- Guidelines for Use of IVC Filters in Treatment of Venous Thromboembolism (SIR, 2020)
- ASCO Guidelines for Prevention and Treatment of VTE in Cancer Patients (2019)
- ASH Guidelines for Diagnosis of VTE (2018)
- ASH Guidelines for Optimal Management of Anticoagulation Therapy for VTE (2018)
- ESA Guidelines for VTE Prophylaxis in Elderly Surgical Patients (2017)
- ACCP Guidelines for Prevention and Treatment of Thrombosis (2012)
- AAOS Guidelines for Prevention of VTE in Hip and Knee Arthroplasty (2011)
- ITAC Guidelines for Prevention and Treatment of VTE in Cancer Patients (2013)
- Additional Resources
- Show All
- Medication
- Questions & Answers
- Media Gallery
- References









