LOS ANGELES — Home telemonitoring of blood pressure (BP) and nurse case management have each proven valuable to reduce hypertension in previous studies. Now, for the first time, researchers demonstrate that combining these strategies in black and Hispanic stroke survivors is linked to a significant drop in systolic BP vs home telemonitoring alone.
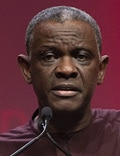
Gbenga Ogedegbe, MD, MPH (© 2020 American Heart Association/Photo by Todd Buchanan)
At 12 months, compared to baseline, the dual intervention group experienced a 14 mmHg drop in systolic BP vs a 5 mmHg decrease in the telemonitoring only group.
The findings are particular noteworthy because the study population had multiple health and socioeconomic risk factors, lead study author Gbenga Ogedegbe, MD, MPH, said at a late breaking abstract session here at the International Stroke Conference (ISC) 2020.
"We strongly believe that these findings provide strong empirical evidence for the widespread implementation of these strategies in low-income, minority stroke survivors with multiple comorbidities."
A High-Risk Population
"As you probably know, blacks and Hispanics have poorer stroke outcomes than Caucasians . . . and hypertension is major predictor of racial disparities in stroke outcomes in the United States," said Ogedegbe, director of the Division of Health and Behavior and the Center for Healthful Behavior Change, Department of Population Health, NYU Grossman School of Medicine in New York City.
Improving hypertension control could therefore be essential to secondary stroke prevention, he added.
Ogedegbe and colleagues enrolled 450 black and Hispanic stroke survivors with uncontrolled hypertension in a multicenter study. They recruited participants at six public hospitals and three academic medical centers "where mostly low-income minority patients in New York City receive care," he said.
Average patient age was 62 years and 44% were women. In addition, 72% of the cohort had an income less than $25,000 per year, "which, as you can imagine, is a very low-income population."
Furthermore, 45% of the study population was obese, 48% had a diabetes diagnosis, and 30% currently drank alcohol. At baseline, almost one third had three or more comorbidities.
Baseline systolic BP was similar between groups, with a mean 150 mmHg in the dual intervention cohort and 148 mmHg in the single intervention arm.
Researchers randomly assigned 224 participants to the dual intervention strategy and another 226 to home telemonitoring only.
In their telephone counseling, nurses addressed lifestyle behaviors and strategies to improve hypertension.
Significant Differences Emerge
The change in systolic BP from baseline to 12 months, the primary outcome, dropped by 14.76 mmHg in the dual intervention group compared to 5.53 mmHg in the single intervention arm. The difference was statistically significant (P < .0001).
Ogedegbe and colleagues also measured 6-month results. At this time, systolic BP had dropped by 13.63 mmHg in the dual intervention cohort vs a 6.31 mmHg decrease in the home monitoring only group (P < .0001).
At both 6 months and 12 months, the between-group differences in systolic BP reduction favored the dual intervention. At 6 months, the difference was 7.32 mmHg and at 12 months it was 9.24 mmHg (P < .0001).
Other study outcomes, including the recurrent stroke rate, are still being adjudicated.
However, "the reduction in systolic blood pressure of 14 mmHg among these patients would be expected to translate to at least a 20% decrease in stroke deaths and 34% fewer secondary strokes," Ogedegbe stated in a release.
Telephone counseling consisted of 20 calls over 12 months. A pharmacist or other trained, nonphysician healthcare provider could substitute for the nurse care manager in their model of care, the investigators noted.
More research could further support this strategy, Ogedegbe said. "Effectiveness of this intervention in secondary stroke prevention warrants further investigation."
"Major Breakthrough"
"It's a super important trial. To see that striking difference in a patient population that is very high risk for strokes is pretty dramatic," session co-moderator Louise McCullough, MD, PhD, told Medscape Medical News when asked to comment on the findings.
"I think the biggest barrier will be cost of sending this home to patients. But when you start looking at the cost of stroke — it's going to be very cost effective," added McCullough, professor and chair of neurology at UTHealth in Houston.
"We have to really think about how our healthcare system funds this, whether it's hospitals, insurers, or CMS," she noted.
"Clearly this is a major breakthrough for this very at-risk population," McCullough said. "It will be exciting to see the stroke results, because this was just blood pressure."
"This trial really speaks to the importance of new ways of improving blood pressure in the population, and particularly in minority and low-income populations," Mitchell S.V. Elkind, MD, president-elect of the American Heart Association and professor of neurology and epidemiology at Columbia University in New York City, said in a video commentary addressing the results.
The telemonitoring component can prompt advice from a doctor or nurse on how to adjust medication. This type of virtual consultation could spare some stroke patients the need to come to the hospital, "which can be difficult especially for stroke patients, and especially for those who may have fewer resources and lower incomes," Elkin said.
He added. "This was a very big effect, and this we know can have a big effect on clinical outcomes as well."
The National Institute of Neurological Disorders and Stroke funded the study. Ogedegbe, McCullough, and Elkind have disclosed no relevant financial relationships.
International Stroke Conference (ISC) 2020: Late-breaking abstract 19. Presented February 21, 2020.
For more Medscape Neurology news, join us on Facebook and Twitter.
Medscape Medical News © 2020
Cite this: Damian McNamara. New Approach Successfully Lowers BP in Minority Stroke Survivors - Medscape - Mar 06, 2020.












Comments