This transcript has been edited for clarity.
Molly Heublein, MD: Hi. I'm Dr Molly Heublein. Welcome to Curbsiders Teach, our Curbsiders family podcast on teaching in medical education.
Era Kryzhanovskaya, MD: I'm Dr Kryzhanovskaya. We're excited to recap one of our favorite episodes from Curbsiders Teach Season 2, Teaching a Physical Exam with Dr André Mansoor.
Heublein: This was such a great one. Dr Mansoor is clearly passionate about the topic and shared some great examples of just how powerful the physical exam can be. We love to rely on technology in medicine, but sometimes the exam can be even more powerful to save patients' time and get to the right diagnosis. Showing our learners how valuable the exam can be is really key. As educators, we need to debunk the myth that physical examination is not helpful.
Kryzhanovskaya: I remember after this episode, I started more consciously paying attention to the physical exam — the patient's' nail beds, pulses, heart sounds, uvula, and other parts of the exam that André highlighted for us. Recently, I was looking at a patient's hands based on the chief complaint and the diagnosis I was considering. I noticed an unexpected nail finding. After scratching my head for a while and generating some hypotheses, André's voice popped into my head. The plaques on the patient's hands were psoriatic arthritis. The oil drop sign came into my awareness. It was truly wild, and I think it was entirely due to our conversation with André.
Heublein: And there is no good blood test or scan we can order to confirm that, so it really is just finding it on an exam. I had a great one yesterday when I was presenting in clinic. One of my favorite diagnoses to make in clinic is BBPV — benign paroxysmal positional vertigo. One of our interns presented this really complex older woman. We were worried that her vertigo could suggest something dangerous. Could it be something central? Eliciting her vertigo with the Epley maneuver was just so satisfying — being able to diagnose the patient based on the physical exam alone and initiate treatment, and reassure them that they don't need more testing.
We're excited about the power of the physical exam. Let's think about how we're actually going to teach this. Dr Mansoor highlighted the one-two punch: teaching the expected findings with a very brief didactic and then going to the bedside to observe them.
Kryzhanovskaya: Let's dive into that a little bit more. André encouraged us to do a little bit of prep to amplify what we're going to see on the exam.
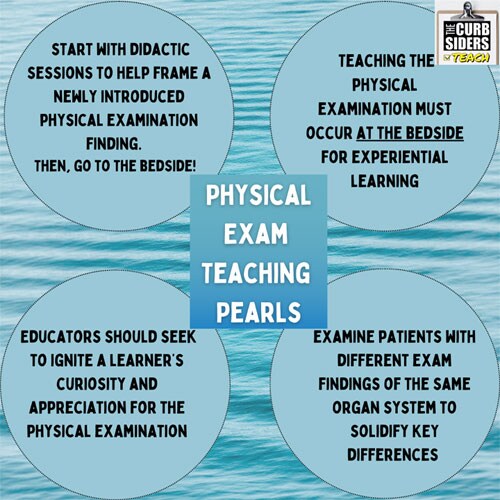
He encouraged us to start with a whiteboard or chalkboard didactic, followed by bedside teaching for kind of that one-two punch. The didactic should be based on the physical exam finding that the learner or team is about to encounter. How do clinicians differentiate those physical exam findings? Having the learners anticipate what they're going to see or hear helps them identify the differential diagnosis for each physical exam finding.
For example, we may go through the defining aspects of the differential for a holosystolic murmur, and the clinical scenarios in which we might hear them. That's where we are performing a hypothesis generating physical exam to help us arrive at the correct diagnosis more efficiently. It saves time for us, for our team, and for the patient as well, and it avoids the kind of shotgun approach of ordering tests immediately and allows us to not overutilize technology or testing.
Heublein: Now that we've set the stage and framed the exam for the learner, we go to the bedside. Think about the learner's experience level and tailor the teaching from there. If you have a newer learner, perform the exam first to model the behavior and then have the learner follow you and describe their findings. If you've worked with a learner for a couple of weeks and you know that last week, you conducted a volume status exam with another patient and you felt like the learner was acquiring those skills, have the learner start the exam and you can give pointers. It's so important to tie the findings to the clinical setting. Have each student describe out loud what they've observed and then talk through the differential diagnosis.
Kryzhanovskaya: Another great tip that André taught us is to solidify findings if possible. Have learners examine patients with different exam findings within the same organ system. For example, with the holosystolic murmur, try to examine patients with diastolic murmurs to solidify the differences in murmurs and other findings in other patients on our teams. We might take the learner to see patients with interesting physical exam findings (after asking the patient for permission) and to get a sense of what findings those other patients might have. It's the hypothesis-driven physical exam again. Most patients love to be part of the teaching experience.
Heublein: I wish that when I was in residency, these methods were utilized more because it's an amazing way to see things in practice and learn on the go. During our podcast, we had a fun walk through, a case of a heart murmur with Dr Mansoor, so I would encourage you to take a listen to the podcast and check out his website, Physical Diagnoses CPX. You will find a wealth of information on ways to improve your teaching of the physical exam — cases you can go through on your own or with your learners to reinforce those findings.
Another tip from Dr Mansoor was for educators who are trying to improve their physical exam skills isget better at teaching the exam is to have a physical diagnosis buddy. If you see something that you're excited about in clinic or on the wards, text or call your buddy and say "Hey, let's go check out this patient together and learn together around this case."
You can listen to the entire podcast here, and see our show notes and graphics as well. I'm Dr Molly Heublein.
Kryzhanovskaya: And I'm Dr Era Kryzhanovskaya. Thanks for joining us on this quick refresher of the physical examination skills episode with Dr André Mansoor as part of Curbsiders Teach, season 2.
Follow Medscape on Facebook, Twitter, Instagram, and YouTube
Medscape Internal Medicine © 2022 WebMD, LLC
Cite this: Teaching the Physical Exam: Best Practice - Medscape - Nov 09, 2022.




Comments