This transcript has been edited for clarity.
Joseph Mikhael, MD: Hello. My name is Dr Joseph Mikhael and welcome to Medscape InDiscussion: Multiple Myeloma. Today, we're talking about future therapies in multiple myeloma. I've had the privilege of being involved in myeloma and myeloma research for over 20 years now. And I have to say, I don't know if there has been a more exciting year in myeloma research than where we are right now. We think of immunotherapy being huge in cancer in general, but in multiple myeloma, it has really changed the way we think about this disease and treat it. We've already seen monoclonal antibodies and antibody drug conjugates and even CAR T-cell therapy make its way into the treatment paradigm for multiple myeloma. But today, we're going to look a little bit into the future to see what is coming. And I can't think of a better guest to join me to discuss the future of multiple myeloma than a world expert on myeloma and also a very dear friend, Dr Nina Shah, who is a professor of clinical medicine in the Department of Medicine at the University of California, San Francisco. Nina, always a pleasure to share the mic with you.
Nina Shah, MD: Thank you so much for having me, Joe.
Mikhael: It's a pleasure. Nina, I mentioned that you are well poised to have this discussion because you have been a huge part of a lot of the clinical trials and a lot of the efforts that are going on right now in the future of myeloma care. I want to start by talking about a patient I saw in clinic today. This patient came to me after they were online reading about myeloma. She had gone to myeloma.org and various other places to learn about the disease. She asked me an interesting question. She said, "I know that I'm still early in my treatment now, doc, but in the future, do you think I'm going to get CAR T-cell therapy or do you think I'm going to get a bispecific therapy?" With that in mind, I'd like us to talk a little bit about these topics. We've talked about CAR T-cell therapies as part of our current standard, and at the end of this discussion, I'd like to see what you think about the future of CAR T-cell therapies. But in the short term, possibly even in the next few months, we may have our first bispecific therapy approved. First of all, Nina, for our audience who's listening, can you give us a quick primer? What are these bispecifics, and how do they work?
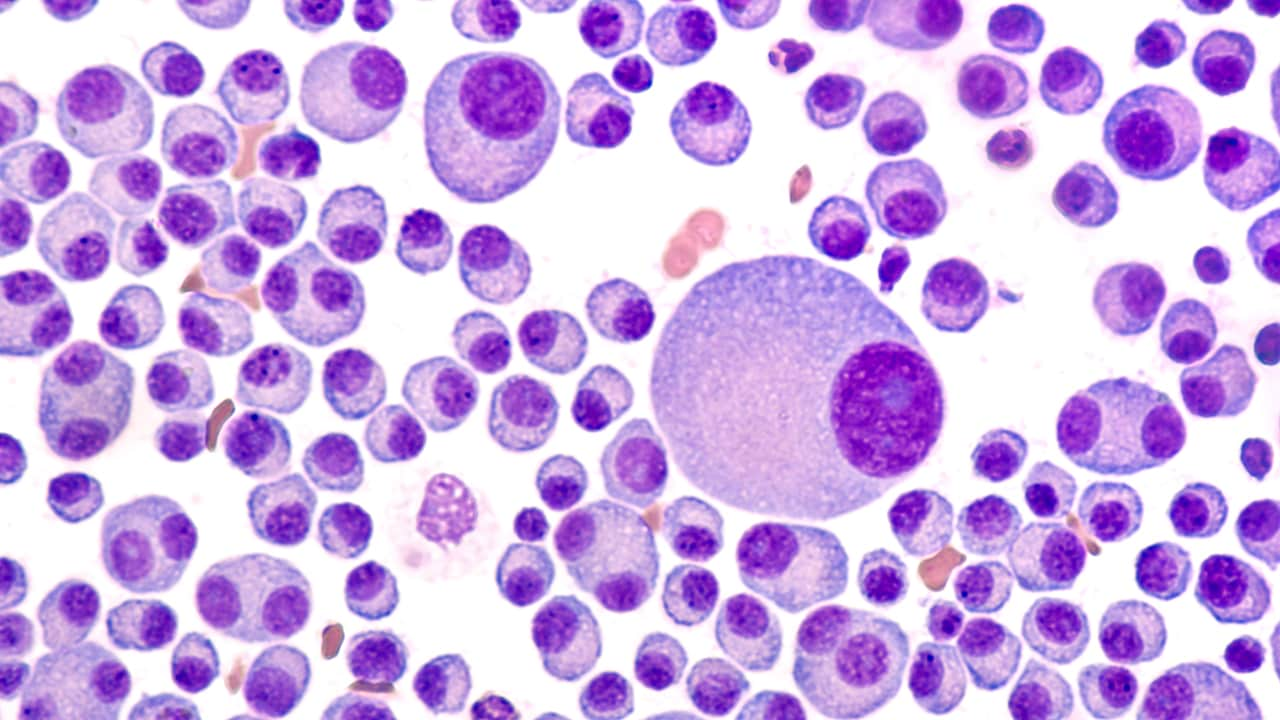
Shah: You've brought up some really good points. Bispecifics are poised to change the way we approach myeloma patients in some regard. For background information, bispecific T-cell engagers are just that; they're a molecule that's off the shelf. So that is a key criteria here — one part of it binds to an antigen or a protein on the surface of the target cell. In this case, the myeloma cell and the antigen often can be BCMA (B-cell maturation antigen), or there are others that we can talk about. And then the other part of it binds to CD3 on the T cell. So it's a way to bring the patient's own endogenous T cells, together with the tumor cells to make them proximal to each other. I always call it the eHarmony of immunotherapy in multiple myeloma — bringing the two things together, so the T cells can have an effective effector response toward the target cell.
Mikhael: So, it's sort of an eHarmony gone bad because the T cell is not exactly going to love on the myeloma cell right now. It's designed to kill the cell. A point you made that is particularly important, before we dive into what we've seen for results of the bispecifics, is the fact that it's off the shelf. One of the exciting things we've seen with the introduction of CAR T-cell therapy into the clinic is that we have unprecedented response rates both in depth and duration of that response, albeit with some toxicity that we discussed, of course. But a lot of patients just don't get access to CAR T-cell therapy geographically, or even because of their frailty or inability to receive some of the chemotherapy. How important is the off the shelf concept that you can just deliver the therapy? While we're talking about this, where do we deliver it to? Patients still need to be admitted [to the hospital] for bispecifics right now.
Shah: These are really good points because although I did say the term "off the shelf," it's "off the shelf" with an asterisk. What I mean is that if this becomes available, which we hope it will this year, people would be able to order it. Doctors can order it and have it infused. However, it is true that there's a 60%-80% chance the person will have cytokine release syndrome, or CRS. Remember, this is a T-cell engaging therapy, and so we expect this, and the CRS tends to be very minimal grade 1 or 2 and very manageable by tocilizumab and/or steroids. We've become accustomed to doing this in the clinical trials. That being said, because there is a 60%-80% chance of this happening, it's important for patients who are going to get this therapy to be monitored in somewhat of a setting. So it's either going to be done in a nice outpatient setting that has easy access to inpatient admission if necessary, or maybe the first one to two doses, including step-up dosing, would be done in an inpatient setting. For this, there is that extra step where there might be a referral to a specialty center or maybe an admission to a hospital — one extra step that isn't completely off the shelf. You can get this without having to plan for things like cell collection, apheresis, etc. But you do have to plan for these things with CAR T-cell therapy, for example.
Mikhael: For the community oncologists listening today, this isn't just another monoclonal antibody where there is a potential for infusion reaction. This infusion reaction, the cytokine release syndrome, obviously is significant enough that it may require hospitalization. Right now, all of the protocols mandate admission to the hospital for at least the first dose, if not the first two doses. But in the future, do you think there's a possibility of developing a bispecific or having a regimen such that patients can be given it entirely in the outpatient setting?
Shah: That's actually the next phase of bispecific research. Right now, we have research looking at just the raw efficacy and safety of these agents, which has been remarkable. But the next phase is how we make it a real-world option for patients. We cannot just have them at a very specific centralized academic center because not a lot of patients can get access to this. Even a hospital connected with a large cancer center in the community is not always possible. What I think the next wave is for us to develop as myeloma specialists is a way to have a workflow for these patients to get the bispecific in the community. One of the things we've been thinking about, even in our own practice, is whether it is possible for patients to get the bispecific as an outpatient, potentially just take one dose of low-dose dexamethasone after the first fever, manage the symptoms at home, and come in to be monitored the next day. This would allow patients to not have to be admitted. We really want to test this to see if we can have the same outcomes — the same good efficacy outcomes — we've seen in the initial trials. These are all the things we hope get studied, so we can provide more information not just to the patients in clinical trials but to the patients who will receive it in the community in the future.
Mikhael: That's such a critical point. One of the barriers to CAR T-cell therapy is having to go into a larger center, get the apheresis, and wait 4 weeks to be reinfused to have the chemotherapy before the reinfusion. It would be ideal if we could give it out in the community. I see a lot of education on CRS coming in the near future. Hopefully, as we get better at managing CRS, even though you said 60%-80%, such a small fraction of patients, have higher grades of CRS — grade 2 or maybe rarely grade 3. Hopefully we can reduce this. The other thing that is interesting, looking to the future in this realm, Nina, is some of the NK or natural killer cell engager bispecifics we're working with. I have a clinical trial open now where we're looking at this, and the hope is that there may be considerably less CRS because it's engaging a NK cell instead of a T cell. So, we've talked about the modality. Let's talk about the brass tacks here. In the triple-class refractory space of myeloma where we have seen proteasome inhibitors, immunomodulatory drugs, and monoclonal antibodies — we've seen very great drugs approved with response rates pretty much between 25% and 30%. We talked about almost tripling that with CAR T-cell therapy. But talk to me about how effective these bispecifics are. Are they in that 25%-30% ballpark? Are we going higher than that?
Shah: This is another remarkable thing about bispecific T-cell engager therapy. It's having response rates somewhere around 60%-80%. So, I always say "60 is the new 30." And that's true because we're talking about single-agent activity — no combination therapy. In phase 1 trials and in the RP2D (recommended phase 2 dose) expansion cohorts, we're seeing 60%-80% response rates and some deep response rates and sustained MRD (minimal residual disease) negativity. These [response rates] are all getting to the top of trying to get really good, deep responses for myeloma patients, which we hope will be reflected in an extended duration of response, although we don't have all of these data available yet. So we are talking about a new era of therapeutics that really raises the bar for what we would expect in this very heavily pretreated patient setting.
Mikhael: It's a little early to talk about the longevity of those responses, but obviously, it's a pretty impressive depth of response. Now, let's talk a little bit about the fact that even for those of us in the field, it's hard to keep track of all the bispecifics. I figure we have at least ten that have been presented at scientific meetings and a whole series of others that are being developed. But when you look at this whole glut of bispecifics, Nina, how do you divide them up in your head? Do you go by target? Do you go by frequency of use? How do you make sense of all these bispecifics?
Shah: It's a really interesting thing that makes for a really nice table, as you can imagine. The first thing I think about is the target. Most of the bispecifics that have been presented so far are targeting BCMA. So we'll put that aside for one second. Then there are two other targets that have been explored. One of them is GPRC5D, and the other one is FcRH5. Those are sort of in a separate category. Now when you think about the BCMA bispecifics, differentiating between all of them is difficult because they're all doing pretty well. They are all fairly safe with very minimal neurotoxicity. We didn't talk about that, but it's actually very minimal. This makes all of them seem that they're on a level playing field. What differentiates each from another are things like route of administration and frequency of administration. We know that some of them are subcutaneous, which some people like because they don't want to get an IV, and others are IV but may be given less frequently. What is going to be interesting is that if we really get a long-term duration of response for these very effective agents, people are going to stop wanting to come every week. They will want to do something else. The whole point of these therapies is for people to have life — not just extended life. They don't want to be going to their oncologist's office every week. There is going to be a nice play for those agents that can extend the interval in between the infusions because that's more of what we've been used to with myeloma therapies; for example, with anti-CD38 antibodies. Patients might want to get a port and just get IV therapy every 3 weeks. We'll see what happens. It's the logistics that's going to differentiate them.
Mikhael: That's going to take some time to sort out. And I know some of them are looking at more intensive treatment early on, kind of like we're doing with some of the CD38s now, and then backing off with time. That will be an important phenomenon. While we're still on the bispecifics for just a little bit longer, help me understand — you mentioned the three different targets, and I know it feels like we've got license plates here for targets: GPRC5D, FcRH5, and BCMA. if you have a patient that has had BCMA-targeted treatment, maybe with belantamab or maybe even with CAR T-cell therapy with ide-cel or cilta-cel, and their disease is now progressing, what do you think about going from BCMA to BCMA?
Shah: This is a great question because we don't have all the data, and I commend a lot of the investigating authors for looking into these pre-BCMA or prior–BCMA-treated cohorts. And there are some now on the various BCMA bispecifics. What we know is that people who have been treated with anti-BCMA agents may still respond to BCMA-directed therapy. That is, there's not necessarily a loss of BCMA on the target. That's not always true. But there are cases where patients still have BCMA therapy and can change modalities; for example, CAR T-cell therapy to bispecific T-cell engager therapy, in order to get efficacy. That being said, if someone's disease had progressed after a BCMA-directed CAR T-cell therapy, especially if it had been a long time, I probably would consider targeting GPRC5D, for example, with talquetamab, which is also a T-cell engaging bispecific therapy. So it's a little bit dealer's choice. The talquetamab data and the cevostamab data — cevostamab targets of FcRH5 — did have cohorts, around 20% here and there, that had prior BCMA therapy. I'd like to look at those data and see what it is. They are small numbers, but at least it helps us to understand beyond BCMA what we may do for these patients.
Mikhael: It's really important as we go forward to understand BCMA resistance a little bit better. It seems you wouldn't go immediately from one CD38 to another. I think we've shown this pretty unequivocally. But with BCMA therapy, there may be less of that. More BCMA may still stick around after a BCMA therapy. So overall, thinking about these bispecifics, it sounds like this is going to be a big wave or maybe multiple waves over the next several months to years. Hopefully within several months, we will have access to a bispecific therapy, which from your estimation sounds like initially will still require admission to the hospital, but with time can be delivered in an outpatient setting. Let's move off bispecifics for a minute, Nina. Let's think about what other novel molecules are coming in multiple myeloma. I know sometimes we get so awed by what's happening with bispecifics, we forget some of these others. Let's talk about the CELMoDs for a minute. What can you tell me about CELMoDs?
Shah: So, CELMoDs are a great way to try to target the myeloma cell, taking advantage of what the cell depends on, which is this intracellular signaling cascade. Ultimately, the garbage disposal of a cell has to function correctly. When that's disrupted, either by a proteasome inhibitor or more proximately some signaling cascade with CELMoDs, you can really target the myeloma cell and not have your traditional chemotherapy side effects. So these are very important drugs. And of course, the prior generations would have been the iMiDs (immunomodulatory drugs) — lenalidomide and pomalidomide. But now we have things like iberdomide. And I will say that one of the advantages about these is that they're oral. That's great, right? Because again, people don't want to spend all their time at the oncologist's office. We've now seen data from the iberdomide studies with the iberdomide combination with dexamethasone, again in that 30% response rate — you know, old school response — but it's still there, and a lot of people were very heavily pretreated in those trials. I want to point out that the toxicity data in that trial are actually very good, and the anecdotal toxicity reports from the investigators are encouraging. For anybody who's used long-term lenalidomide, it can be a little bit difficult for patients to stay on it. If we could find an iMiD that works in lenalidomide-resistant patients and is well-tolerated with not as many low blood cell counts, diarrhea, fatigue, et cetera, it would be a real win for our patients. I'm looking forward to seeing what iberdomide does. There are data to come by iberdomide with daratumumab or bortezomib. Those are the next-phase trials that are already reading out now. And there's a possibility of having iberdomide now after CAR-T cell therapy, which is the plan for a lot of trials. It would be interesting to see what the immunostimulatory effects are of that because there are correlative data to suggest it's having a better effect on the immune system than even lenalidomide. So, it will be a nice way to see if you could combine CAR T-cell therapy and iberdomide.
Mikhael: Well, that's fantastic. It's quite striking, isn't it? We're going from this one extreme of CAR T-cell therapy with all of the complexities of the process and even bispecifics to just a straightforward pill like these CELMoDs in a disease we've yet to cure. In a disease that can present in so many ways, from extremely aggressive to less aggressive, it's really nice to have different tools in the toolbox. CELMoDs will have a place. There will be that time where people will want just a relatively straightforward pill. And as you've said, with less toxicity than we've seen before in the iMiDs, it could be really attractive. Have there been other molecules you've had an eye on? I know there have been a couple of interesting presentations of modakafusp. First, I know sometimes it's hard to pronounce that. You're too young, but I'm old enough to remember the early days of myeloma where we used interferon. Now it seems like they've brought back interferon to the world of myeloma in this modakafusp. What do you think about it?
Shah: It's basically targeted delivery of cytokine, right? Because they take advantage of the CD38, it is something that is really putting together our ideas of targeting plus our ideas of immunostimulation. They did have some very nice data this year presented at the American Society of Hematology (ASH) meeting that suggested there could be responses, again in the 20-30s — the early response rates. This is something we could think about as far as combining with other therapies, as well. Again, with these immunostimulatory sort of therapies — the cytokines, and even the CELMoDs — we have a chance to think about them not just as their own drug, but if they could be a good partner for the existing awesome immunotherapies like CAR T-cell therapies and bispecifics. My hope is to go into a steroid-free zone with combining all of these things because it tries to limit the drug that a lot of patients just hate.
Mikhael: I agree with you. I was having a conversation today with a patient about how I joke that I want to change the name of the myeloma service to the Dexamethasone Reduction Service because we so often have to do that. I always tell patients it is like booster rockets on the shuttle — really good for initial launch but not when we want them to go down. It raises the issue, obviously, of the quality of life of the patient. One of the real draws to CAR T-cell therapy is this one-and-done–like concept where patients can have their treatment and then go off all treatment. Our ultimate goal is to find a way to get people off all treatment. I'm hoping that some magic combination of all of these different things we've described with the big guns of CAR T-cell therapy, other treatments like the bispecifics, something as simple as the oral medications like CELMoDs, or something like modakafusp could give us that sweet spot where we can get the disease down long enough and deep enough so patients can come off treatment. Before we wrap up, Nina, there's a third area I want to think about. We talked about bispecifics. We talked about some of these novel molecules. I know we already have CAR T-cell therapy available in myeloma, but as with any great modality, this is still the early voyage. How do you see the future of CAR T-cell therapy? Not so much using the ones we have now maybe in earlier therapy lines — we had some discussion about that earlier — but what do you see with other forms of CAR T-cell therapy? Are we going to be using CAR T cells that don't only target BCMA? Are we going to be using CAR T cells where we don't have to collect T cells from the patients? Could that holy grail of off-the-shelf CAR T-cell therapy be something that's actually real? What is your take on that for the future?
Shah: In response to your first question, there are CAR T cells being developed not just against BCMA. Particularly, the GPRC5D-targeted CAR T cell has been developed both by an industry partner and Memorial Sloan Kettering with their investigator-initiated study, which actually had a very good amount of pre-BCMA people who had been treated with BCMA therapies before. We got some nice data from them, and it [the GPRC5D-targeted CAR T cell] seems to be well tolerated, which is great. This will be another option for patients. Maybe they've had a bispecific that targeted BCMA, and then they can go to a GPRC5D-targeted CAR T-cell therapy or vice versa. So that's one option. Your point about apheresis is so important. A couple of years ago, I wouldn't have even thought that AlloCAR T could be something that's a player. But I think if we can get it right for AlloCAR T off the shelf, it will be something that really is a competitor in the space. The reason for this is that it eliminates that entire apheresis workflow, which is literally a workflow. You have to get patients in, they have to be there for a couple of days, and they have all the testing. It's like with the first part of the transplant with the stem cell collection — not exactly the same, but it takes up space, that is, you can't replace it. You need that space, and it not only takes up space at your institution, but it also takes up space on the manufacturing side, which is from the industry partner. So that is limited. You just can't create a bunch of CAR T cells if they're autologous. So if allogeneic CAR T-cell therapy could be something that's safe — and I think it can be done safely now that we have engineering strategies to take out the T cell receptor — the challenge will be the efficacy. Those allogeneic CAR-T cell therapies will have to come in and do every single piece of work they can in that first 30 days when there's true lymphodepletion. Because of course, as the patient's own immune system starts to grow back, there will be this likely rejection of the CAR T cells. We really hope we can get better at target modification, or targeted discovery I should say, to get the right target or target combinations to have a deep response in that first 30 days, so we can ride that wave and yet not have to send the patient to receive apheresis.
Mikhael: That's fantastic. I love the idea of having more ways to approach myeloma. Every patient is different. Every patient is unique, as we've said; sometimes we can do something as intense as a conventional CAR T-cell therapy. Other times, we just want to use oral therapy. It really seems that the future of myeloma is bright and that lots of things are coming. Well, Nina, I really want to thank you for taking time with us today. It's always a pleasure to chat with you. In summary, we have seen a little glimpse into the future of multiple myeloma, and in the very near future, we're almost definitely going to have access to bispecifics. It appears that several of them are in development and are on the way. Whether they target BCMA, GPRC5D, or FcRH5, we're going to be able to use the principles we have from CAR T-cell therapy in a more easily deliverable way and hopefully in a way, with time, that it can be done exclusively in an outpatient setting. We have other novel molecules like CELMoDs and modakafusp that may also have a significant role either by themselves or in combination with others. There is hope indeed that we may be able to deliver CAR T-cell therapy in a more easily deliverable fashion and maybe even off the shelf with AlloCAR T. I know we haven't covered everything, Nina. There's a lot of other great research and still so much to come with how we sequence all of these. We have got a lot of work to do, but I'm very excited about the future of myeloma, and I really appreciate you taking time today to share this with the listeners and me. Thank you very much, Nina.
Shah: Thank you. This was really great, and I appreciate you having me.
Mikhael: It's a pleasure. And we trust that those listening today will benefit from this as they care for your patients. Thank you very much.
Resources
International Myeloma Foundation
CAR T-Cell Therapy for Multiple Myeloma
Bispecific Antibodies Versus CAR T-Cells in Multiple Myeloma Treatment: Pros and Cons
Bispecific Antibodies With Multiple Targets Moving Forward in Multiple Myeloma
GPRC5D Is a Target for the Immunotherapy of Multiple Myeloma With Rationally Designed CAR T Cells
A Study of Talquetamab in Participants With Relapsed or Refractory Multiple Myeloma
Molecular Mechanisms of Cereblon-Interacting Small Molecules in Multiple Myeloma Therapy
A Phase I Study of MCARP09 and MCARP25 CAR T-Cell Therapy in People With Multiple Myeloma
Follow Medscape on Facebook, Twitter, Instagram, and YouTube
Medscape © 2022 WebMD, LLC
Any views expressed above are the author's own and do not necessarily reflect the views of WebMD or Medscape.
Cite this: Multiple Myeloma Therapies: A Glimpse Into the Future - Medscape - Aug 10, 2022.








Comments